The Centre
Non-communicable Diseases (NCDs) are those that do not pass from person-to-person and include long-term conditions.
Worldwide, they cause 8 out of 10 premature deaths, with the burden greatest in low and middle- income countries. This includes countries in Latin America, where long-term NCDs are a leading cause of disability and poor quality of life. Across Latin America, long-term conditions are treated in expensive hospital services as there is a lack of quality community-based care to help people manage their condition.
The NIHR Global Health Research Centre: Community Management of Non-Communicable Diseases in Latin America aims to strengthen research and service capacity, conduct high quality research and ultimately improve quality of life and disease specific outcomes for individuals with long-term NCDs, including those from often neglected indigenous communities. The Centre will be regional, with sites in Bolivia, Colombia and Guatemala. Researchers from Latin America with expertise in a range of areas including family medicine, mental health and community treatment will work in collaboration with UK experts to set up and support the Centre.

Supported by Queen Mary University of London (UK), the Centre will link a leading university in Colombia, Universidad Javeriana, as a regional hub with two universities namely in Bolivia (Universidad Franz Tamayo) and Guatemala (Universidad Rafael Landívar).
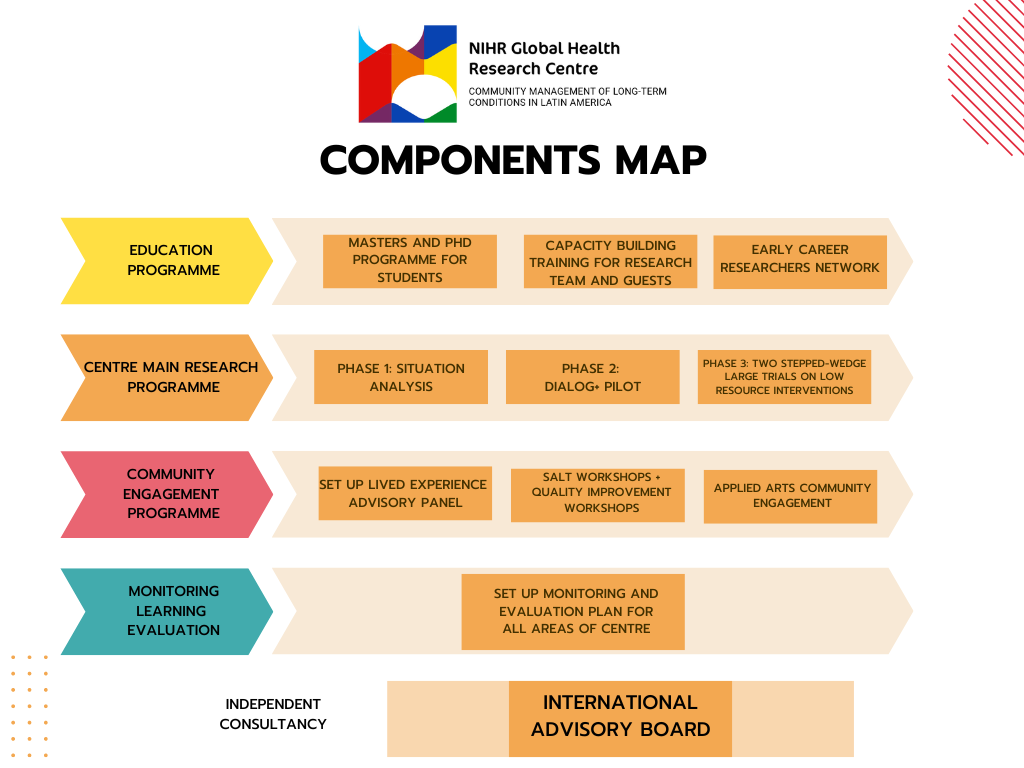
Key Programme Areas
The Centre will address the most prevalent classes of NCDs within Latin America: Diabetes, Cardiovascular Diseases (CVD), Chronic Respiratory Diseases and Mental Disorders. Preparatory work with stakeholders will be followed by pragmatic trials, blending effectiveness research with real-world implementation to maximise sustainability and impact. Broadly, the research conducted will focus on improving community treatment via resource-oriented interventions that influence health behaviours, reduce modifiable risk factors and shift attitudes.
Rather than aiming to establish new expensive services, these interventions are low-cost and utilise the existing personal and social resources available to patients, their families and within the wider community. We will focus on what can be changed and implemented within the community and on low-cost evidence-based interventions that can be applied alongside basic services.
- Situation Analysis: This will include an exploratory Situation Analysis phase, to access resources and challenges on the pathways of care for each country.
- Pilot: Followed by the conduction of pilots of low-resources interventions on three sites, such as 1) DIALOG+, an easy to train IT-supported method to improve the effectiveness of routine consultations; 2) multi-family groups; 3) peer support and 4) volunteer befriending by non- professionals with groups of patients. All of the approaches utilise and strengthen existing resources, including social networks and community support, and have the potential to reduce modifiable risk factors, including those common across different NCDs.
Stepped-Wedge Trials: As a final stage, we’ll test effectiveness of the interventions in two large-scale Hybrid II trials. One will focus on Diabetes, CVD, Chronic Respiratory Diseases as three highly comorbid conditions with some common and modifiable risk factors, with subgroups for each major included NCD. The other trial will address Mental Disorders with subgroups for major disorder categories. Hybrid II trials enable estimating effectiveness whilst ensuring the research remains pragmatic and addresses implementation in practice13. Both trials will be conducted in urban and rural regions, including areas with large indigenous populations
The Centre’s comprehensive capacity-strengthening programme uses a research-driven approach, where the research activities provide the framework and learning environment for the training strategy. The studies will consolidate learning from the taught courses and workshops. We will focus on three areas identified as key to strengthening the capacity required for sustainable and competitive research:
- Fully funded PHD and Masters degrees within a programme of postgraduate training developed by the Colombian site. This will provide a career pathway for the most talented and committed students within the LMIC institutions.
- A regional network of Early Career Researchers (ECRs) to foster collaboration between partners, develop the next generation of research leaders, and establish a critical mass of experts within the region.
- Acomprehensive workshop and training programme led by the sites in Colombia and the UK addressing research methodology, resource-orientation and professional support services. This will cover key skills gaps identified by the sites in Bolivia and Guatemala.
The Centre will be co-created in collaboration between the sites in Latin America and the UK, representing a shared vision across the partner organisations. An effective communication strategy will ensure that all members are equitably involved in decision-making processes, and that outputs will reflect a fair and appropriate acknowledgement of contributions. The equitable partnerships go beyond the academic institutions and involve different stakeholders including people with long-term NCDs and mental health, individuals from rural and indigenous communities, family members, clinicians, managers and policy makers. Stakeholder advisory groups will inform priorities, procedures and public engagement activities.
Throughout, we will engage with community members as active stakeholders. Engagement activities will centre on participatory methods, including establishing advisory boards, hosting interactive workshops and utilising innovative dissemination methods.
Throughout the development of the centre a Monitoring, Learning and Evaluation plan will be developed and implemented, taking into account key indicators, qualitative and quantitative approaches to review, measure and calculate impact of core activities and programmes.


Research Centre: Visual Map of Content